The history is a crucial step in diagnosis of headaches (Table 1.1). A separate history is required for each type of headache reported, in particular noting the course and duration of each. The International Headache Society has developed classification and diagnostic criteria for the majority of primary and secondary headaches (Box 1.1). Although this is primarily a research tool, standardized diagnostic criteria have helped to ascertain headache prevalence, which is useful for understanding the likelihood of any headache presenting in clinical practice (Tables 1.2 and 1.3).
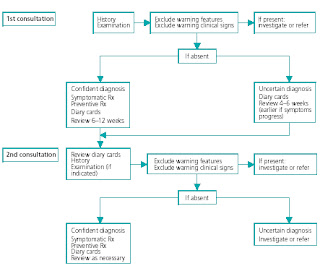
A headache history requires time. In the emergency setting particularly, there may not be enough time to take a full history. The first task is to exclude a condition requiring more urgent intervention by identifying any warning features in the history (Box 1.2).
Box 1.1 The International Classification of Headache Disorders (2nd edition)
Primary headache 1. Migraine, including:
• Migraine without aura
• Migraine with aura
• Childhood periodic syndromes that are commonly precursors of migraine
• Cyclical vomiting
• Abdominal migraine
• Benign paroxysmal vertigo of childhood
2. Tension-type headache, including:
• Infrequent episodic tension-type headache
• Frequent episodic tension-type headache
• Chronic tension-type headache
3. Cluster headache and other trigeminal autonomic cephalalgias, including:
• Cluster headache
• Paroxysmal hemicrania
• Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing
4. Other primary headaches, including:
• Primary cough headache
• Primary exertional headache
• Primary headache associated with sexual activity
• Primary thunderclap headache
Secondary headache
5. Headache attributed to head and/or neck trauma, including:
• Chronic post-traumatic headache
6. Headache attributed to cranial or cervical vascular disorder, including:
• Headache attributed to subarachnoid hemorrhage
• Headache attributed to giant cell arthritis
7. Headache attributed to non-vascular intracranial disorder, including:
• Headache attributed to idiopathic intracranial hypertension
• Headache attributed to low cerebrospinal fl uid pressure
• Headache attributed to non-infectious infl ammatory disease
• Headache attributed to intracranial neoplasm
8. Headache attributed to a substance or its withdrawal, including:
• Carbon monoxide-induced headache
• Alcohol-induced headache
• Medication-overuse headache
• Triptan-overuse headache
• Analgesic-overuse headache
9. Headache attributed to infection, including:
• Headache attributed to intracranial infection
10. Headache attributed to disorder of homoeostasis
11. Headache or facial pain attributed to disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cranial structures, including:
• Cervicogenic headache
• Headache attributed to acute glaucoma
12. Headache attributed to psychiatric disorder
Neuralgias and other 13. Cranial neuralgias and central causes of facial pain including:
Headaches • Trigeminal neuralgia
14. Other headache, cranial neuralgia, central or primary facial pain
Appendix (unvalidated Including:
research criteria) • Pure menstrual migraine without aura
• Menstrually-related migraine without aura
• Benign paroxysmal torticollis
• Headache attributed to major depressive disorder
New or recently changed headache calls for especially careful assessment. New headache in any patient over 50 years of age should raise the suspicion of giant cell arthritis. Headache is likely to be persistent when present, often worse at night and may be very severe. Jaw claudicating is so suggestive that its presence confirms the diagnosis until proved otherwise. In the absence of ‘red flags’, strictly unilateral headaches may suggest a common headache, such as migraine (Chapter 2) or one of the more rare trigeminal autonomic cephalalgias.
An uncommon but avoidable cause of non-specific c headache in elderly patients is carbon monoxide poisoning. This is caused by using gas heaters, which may be faulty, without adequate ventilation. The symptoms of sub-acute carbon monoxide poisoning include throbbing headache, nausea, vomiting, giddiness and fatigue.
The major fear among patients and healthcare professionals is that a brain tumor is the cause of the headache. In practice, intracranial lesions (tumors, subarachnoid hemorrhage, meningitis) give rise to histories that should bring them to mind. It is rare for brain tumors and other serious conditions to present as isolated headache (Table 1.4). Epilepsy is a cardinal symptom of intracerebral space-occupying lesions, and loss of consciousness should be viewed very seriously. Problems are more likely to occur with slow-growing tumors, especially those in neurologically ‘silent’ areas of the frontal lobes. Subtle personality change may result in treatment for depression, with headache attributed to it. Heightened suspicion is appropriate in patients who develop new.
Table 1.2 Lifetime prevalence of primary headaches
Type of headache Prevalence % (95% CI)
Migraine without aura 9 (7–11)
Migraine with aura 6 (5–8)
Episodic tension-type headache 66 (62–69)
Chronic tension-type headache 3 (2–5)
Cluster headache 0.1 (0–1)
Table 1.3 Lifetime prevalence of secondary headaches
Type of headache Prevalence % (95% CI)
Head trauma 4 (2–5)
Vascular disorders 1 (0–2)
Non-vascular cranial disorders 0.5 (0–1)
Substances or their withdrawal (excluding 3 (2–4)
hangover)
– hangover 72 (68–75)
Non-cephalic infection 63 (59–66)
Metabolic disorder 22 (19–25)
Disorders of the cranium, neck, eyes 0.5–3 (0–4)
– sinuses 15 (12–17)
Cranial neuralgias 0.5 (0–1)
Table 1.4 Secondary causes of headache identifi ed in the year after presentation in primary care of a
primary headache or new undifferentiated headache
Subsequent secondary Headache diagnosis at presentation n (%)
diagnosis
New undifferentiated Primary headache
headache n = 63 921 n = 21 758
Subarachnoid haemorrhage 87 (0.14) 5 (0.02)
Malignant brain tumour 97 (0.15) 10 (0.045)
Benign space-occupying lesion 30 (0.05) 2 (0.009)
Temporal arteritis 421 (0.66) 40 (0.18)
Stroke 678 (1.06) 97 (0.45)
Transient ischaemic attack 273 (0.43) 54 (0.25)
Box 1.2 Warning features in the history warranting investigation
• Acute thunderclap headache (intense headache with abrupt or ‘explosive’ onset)
• Headache with atypical aura (duration >1 hour, or including motor weakness)
• New onset headache in a patient younger than 10 years or older than 50 years
• Progressive headache, worsening over weeks or longer
• Fever
• Symptoms of raised intracranial pressure:
drowsiness
postural-related headache
vomiting
• New onset seizures
• History of cancer or HIV infection
• Cognitive or personality changes
• Progressive neurological deficit:
progressive weakness
sensory loss
dysphasia
ataxia